Optional H2 Subhead
Provider Update July 2023
ID Card Updates
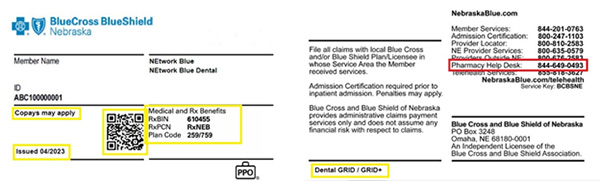
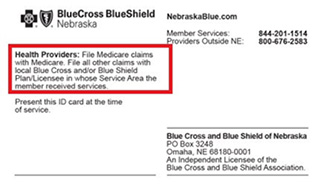
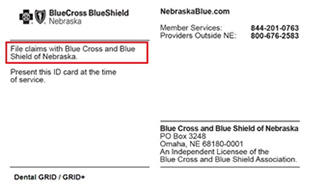
Beginning in July 2023, member ID cards will be updated to a new format. The card's contents will remain unchanged, except for an updated Pharmacy Help Desk phone number for all ID cards as well as the addition of claim filing instructions to Medicare Supplement and dental-only ID cards.
Updated ID cards will not be mass issued; instead, new cards will be issued as members make plan changes that would trigger a new ID card (adding a new member, changing network, etc.) or for new members.
Below is a sample of a new ID card with the format changes highlighted. Items highlighted in yellow are in a new spot; items highlighted in red are new/updated.
Medicare Supplement
Dental
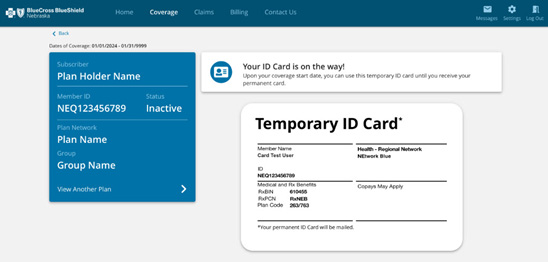
In addition to the format changes, beginning in August 2023, newly enrolled members will have access to a digital temporary ID card. This ID card will only show the member ID number. To verify benefits and eligibility, please log in to Navinet®, call our automated voice system at 800-635-0579, or contact Customer Service.
NaviNet is a healthcare provider portal providing services for Blue Cross and Blue Shield of Nebraska
Changes to Paper Checks and Paper Remits
On May 25, 2023, BCBSNE implemented a change in our mail processing. This change impacts the time it will take for providers not signed up for EFTS and ERAs to receive paper check payments and paper remits.
Previous Process:
Checks and remits were received within 3-5 business days.
New Process:
Checks and remits will be received within 5-7 business days.
As we continue to enhance our digital delivery channels, paper transactions will decrease. To get ahead of future transitions and avoid the extended time it will take to receive the check and remit, providers can sign up for EFTs and ERAs by completing the forms found on NaviNet and submitting to HealthNetworkRequests@NebraskaBlue.com.
- Electronic Funds Transfer (EFT)
- Electronic Remittance Advice (ERA)
If you have questions, please contact your Provider Executive.
Medicaid Redetermination
In March 2020, the Centers for Medicare and Medicaid Services (CMS) temporarily waived certain Medicaid and CHIP requirements. This allowed thousands of Nebraskans to retain their health coverage during the pandemic regardless of any change in status.
Medicaid redeterminations are now resuming, so Nebraska Medicaid and CHIP members could begin losing coverage as early as May 2023. Medicaid members losing their coverage will be eligible for a Special Enrollment Period (SEP) to enroll in an ACA plan. This SEP lasts until July 31, 2024.
Please help your patients understand that they should apply for new coverage before their Medicaid coverage terms. If they wait, they may have a lapse in coverage. Download the Medicaid Redetermination flier to help patients who may have questions about getting coverage.
Coordination of Benefits (COB) Timely Filing
Claims must be received within 120 days of the date the provider received the EOB from the primary payor. Effective June 1, 2023, providers will no longer submit COB information on the Timely Filing forms. Providers will submit COB information as a reconsideration.
Preauthorization Requests
Preauthorization requests are reviewed in a timely manner, based on priority ordered by the provider. The timeline for review is from the receipt of the request to communicating the decision. The timeline is based on accreditation standards and regulatory requirements. Preauthorization requests include Pharmacy, Medical and Radiology.
Priority:
- Non-urgent: Includes up to 15 calendar days to communicate the review decision.
- Urgent: Includes requests ordered by the provider as urgent, meaning the 15-day timeline could seriously jeopardize the life or health of a patient or subject the patient to severe pain that cannot be adequately managed without the requested treatment. When the ordering provider indicates urgent, we communicate the review decision within 72 hours of receipt of the request.
- Step-therapy: Except in the case of an urgent care request and upon receipt of complete, clinically relevant written documentation a review decision is provided within five calendar days.
To ensure most efficient review of the request:
- Use the online preauthorization portal through NaviNet for Medical and Radiology preauthorizations. The review turnaround time is quicker since it eliminates time setting up the request. View the online preauthorization portal at NebraskaBlue.com/Providers/Preauthorization
- Always indicate the correct priority ordered by the provider, per their orders and/or medical records when you submit the preauthorization through the online tool or via a faxed request.
- Always include medical records for clinical review by attaching a pdf document or add a note in the online tool or faxing in the request. If not included, clinical staff will need to request medical records; this delays the clinical review until the records are received to review the request.
- Always include the contact’s name, phone number and fax number in the online portal preauthorization request notes. This is helpful if additional medical records are needed to review your request. If there is no fax number, this will delay the request for medical records.
Always include the following on all faxed requests:
- The complete BCBSNE ID number, including the alpha prefix (this should match what is listed on the patient’s BCBSNE member ID card)
- The complete patient’s name (this should match what is listed on the patient’s member ID card)
- Patient’s date of birth
- Patient’s address, city and state
- Ordering provider’s first and last name (NPI alone is not sufficient)
- Ordering provider’s full address
- Facility/rendering provider’s full name
- Facility/rendering provider’s address
- Contact name, phone number and fax number who submits the request.
- Procedure and diagnosis information
Gold Card Program
Gold Card Program Overview:
The Gold Card Provider program is designed to decrease the administrative responsibilities of the prior authorization process. BCBSNE offers this program to physicians and mid-level providers who meet pre-determined procedure volume and denial metrics when submitting prior authorizations for patients covered by a commercial or Affordable Care Act (ACA)/marketplace health plan. The program applies to the following designated procedures:
- Sinus Surgeries
- Hysterectomies
- Pain management
- Spinal surgeries
The benefits of being a Gold Card provider are:
- Decreased administrative burden for medical review of designated procedures.
- Receipt of automatic authorization with submission of designated procedures.
- Proven increased provider satisfaction.
How to Qualify:
To be considered for the Gold Card program, a provider must perform a minimum of 50 of the specified procedures and maintain an overall prior authorization denial rate of 6% or less in a two-year period.
Participant Evaluation:
- Gold Card status is re-evaluated every 12 to 14 months with an audit of medical records for the designated procedures.
- If the audit reveals a denial rate of 6% or less, Gold Card status will be renewed for another 12 months.
- If the audit reveals a denial rate greater than 6%, Gold Card status will be in a probationary period and re-audited in six months.
- If the denial rate is 6% or less, Gold Card status will be re-instated
- If the denial rate is still greater than 6%, Gold Card status will be terminated. The provider will not be eligible for Gold Card status re-evaluation for two years from termination.
If you would like more information about the Gold Card Program, please reach out to the Provider Executive assigned to your practice. To find out who your Provider Executive is, please view the provider contacts at NebraskaBlue.com/Providers/Provider-Contact.
Provider Directory: Make Sure Your Information is Correct
The Consolidated Appropriations Act (CAA), effective Jan. 1, 2022, requires that online provider directory information be reviewed and updated if needed, at least every 90 days.
All providers, including dentists, can now review directory information in NaviNet. Directory information for your office can be located under Practice Documents.
For PHO groups handling their own credentialing processes, we will be requesting the submission of a full roster every 90 days.
Please take a few minutes to review your online provider directory information to help ensure BCBSNE members can locate your most current information.
If changes are needed, please take the time to update your information by submitting updates and corrections via one of our provider forms on NebraskaBlue.com/Providers/Find-a-Form.
Quality Provider Articles
Manage osteoporosis to limit disability
Musculoskeletal conditions are the leading contributor to disability, according to the World Health Organization.
The Osteoporosis Management in Women (OMW) who had a Fracture (OMW) HEDIS® star measure assesses women 67–85 years of age who suffered a fracture and had either a bone mineral density test or received a prescription to treat osteoporosis within six months of the fracture.
Read the OMW tip sheet to learn more about this measure and the information to include in medical records.
Source: Musculoskeletal health (who.int)
Importance of statin therapy for patients with cardiovascular disease and diabetes
According to the National Committee for Quality Assurance, cardiovascular disease is the leading cause of death in the United States. People with diabetes also have elevated cardiovascular risk, thought to be due, in part, to elevations in unhealthy cholesterol levels. This places people with diabetes at significant risk for developing Atherosclerotic Cardiovascular Disease (ASCVD).
American College of Cardiology and American Heart Association (ACC/AHA) guidelines state that statins of moderate or high intensity are recommended for adults with established clinical ASCVD. The American Diabetes Association and ACC/AHA guidelines also recommend statins for primary prevention of cardiovascular disease in patients with diabetes, based on age and other risk factors. Guidelines also state that adherence to statins will aid in ASCVD risk reduction in both populations.
To learn more about the importance of statin therapy, read the Statin Therapy for Patients with Cardiovascular Disease (SPC) and Statin Use in Persons with Diabetes (SUPD) tip sheets:
Source: Statin Therapy for Patients With Cardiovascular Disease and Diabetes - NCQA
Healthcare Effectiveness Data Information Set (HEDIS®) is a registered trademark of the National Committee for Quality Assurance (NCQA).
Medicare Advantage: Codes Removed from Preauthorization
Effective May 1, 2023, the following codes were removed from the prior authorization list:
| CODE | DESCRIPTION |
|---|---|
| 88271 | MOLECULAR CYTOGENETICS DNA PROBE EACH |
| 88273 | MOLECULAR CYTOGENETICS CHRMOML ISH 10-30 CLL |
| 88275 | MOLEC CYTG INTERPHASE ISH ANALYZE 100-300 CLL |
| 88291 |
CYTOGENETICS&MOLEC CYTOGENETICS INTERP&REP |
| 93241 |
EXTERNAL ECG REC>48HR<7D SCAN ALYS REPORT R&I |
| 93242 |
EXTERNAL ECG REC>48HR<7D RECORDING |
| 93243 |
EXTERNAL ECG REC>48HR<7D SCANNING ALYS W/REPORT |
| 93244 | EXTERNAL ECG REC>48HR<7D REVIEW & INTERPRETATION |
| 93245 |
EXTERNAL ECG REC>7D<15D SCAN ALYS REPORT R&I |
| 93246 |
EXTERNAL ECG REC>7D<15D RECORDING |
| 93247 |
EXTERNAL ECG REC>7D<15D SCANNING ALYS W/REPORT |
| 93248 |
EXTERNAL ECG REC>7D<15D REVIEW & INTERPRETATION |
| S9960 |
AMB SERVICE AIR NONEMERGENCY 1 WAY FIXED WING |
| S9961 |
AMB SERVICE AIR NONEMERGENCY 1 WAY ROTARY WING |
Medicare Advantage: Updates to Carelon Clinical Appropriateness Guidelines
Effective for dates of service on and after Sept.10, 2023, the following updates will apply to the Carelon Clinical Appropriateness Guidelines (Formerly AIM Specialty Health guidelines). As part of the Carelon guideline annual review process, these updates are focused on advancing efforts to drive clinically appropriate, safe and affordable health care services.
Updated Guidelines
Radiology:
- Imaging of the Spine
- Imaging of the Extremities
- Vascular Imaging
For questions related to guidelines, please contact Carelon via email at MedicalBenefitsManagement.guidelines@Carelon.com. Additionally, you may access and download a copy of the current and upcoming guidelines Guidelines.CarelonMedicalBenefitsManagement.com.
Sign up for Navinet®
Registration is free, all you need is a Federal Tax ID. All participating BCBSNE health care and dental providers can enroll for access.
If your office is already using Navinet, please contact your Security Officer to create a Navinet account for you. If you do not have a NaviNet account, please visit
Connect.NaviNet.net/Enroll to begin the registration process.
NaviNet is a healthcare provider portal providing services for Blue Cross and Blue Shield of Nebraska
NaviNet Enhancement: Claim Appeal – Coming in soon!
Coming soon in NaviNet, submitting an Appeal, Reconsideration or Claim Timely Filing Dispute will become even easier!
Those request types will be moving to our new Claim Appeal application. Instead of filling out the forms from our provider website and attaching them to claims to submit your request, you will simply go to your claim status details, click on the  button, and select the Type and Reason for your request. You can add free-form text, attach any supporting documentation (in a PDF format) and submit the request.
button, and select the Type and Reason for your request. You can add free-form text, attach any supporting documentation (in a PDF format) and submit the request.
BCBSNE will respond to your request in NaviNet to let you know when the appeal has been reviewed, if it is being routed to another team and when a resolution has been reached.
If you have any questions about your request while it is in process, you can also use the new Claim Investigation functionality to send an inquiry to BCBSNE, by clicking the  button on your claim. If your request is reviewed and denied, the denial letter will now also be available in the Document Table located directly below the “Claim and Service Line Details” section of your Claim Status Details screen. This new Claim Appeal functionality will be available in NaviNet soon. Additional communication will be provided soon regarding the specific date.
button on your claim. If your request is reviewed and denied, the denial letter will now also be available in the Document Table located directly below the “Claim and Service Line Details” section of your Claim Status Details screen. This new Claim Appeal functionality will be available in NaviNet soon. Additional communication will be provided soon regarding the specific date.
Security Corner: "Security Fatigue"
All the security policies in the world cannot protect sensitive information if your staff is over-burdened by complex, manual security requirements.
Combat “Security Fatigue” amongst your workforce, while allowing them to maintain secure behavior:
- Limit the number of security decisions that staff need to make on their own.
- Make it simple for staff to choose the right security option.
- Design for consistent security decision-making whenever possible.
In the end, the goal should be to make it easier for your staff to be secure than not secure. For more information, visit NIST.gov and search for keyword Security Fatigue.
