Provider FAQs
NaviNet®
Below you'll find answers to the questions we get asked the most.
Registration
Each office must have a minimum of one Security Officer who is responsible for registering with NaviNet, adding users to the account, and granting user access. Your designated security officer should go to https://register.navinet.net to begin the registration process.
- Registration takes between five to seven business days.
- Registration requires a Tax ID and email address.
- Each user will have their own username and password. No sharing is allowed.
- Users have 60 days to log in for the first time before they will become disabled.
- Users should see their Security Officer to have their password reset if they become disabled.
- See the Provider Registration Flyer for more information.
You may check the status of your NaviNet registration at any time from the Registration Page or Help Center.
If you are an existing NaviNet user, and are either a participating BCBSNE network provider, or are a healthcare provider within the state of Nebraska, you should see Blue Cross and Blue Shield of Nebraska as an option in your Health Plans List.
Please verify that the phone number and address you entered when registering for NaviNet matches the phone number and address you have on file with BCBSNE.
If this information is valid and you are still unable to register, please call 888-482-8057 - available Monday - Friday, 7:00 a.m. - 10:00 p.m. CT, Saturday, 7:00 a.m. - 2:00 p.m. CT.
You may check the status of your NaviNet registration at any time from the Registration Page or Help Center.
If a provider’s registration information is accurate, complete, and matches the information we have on file, the NaviNet registration process should take five to seven business days. If anything does not match, NaviNet will attempt to reach the provider by phone for clarification.
Upon initial enrollment, you will get an acknowledgment email from enrollment@navinet.net. Once confirmed, you will get another email with login information and next steps.
Visit the NantHealth Help Center to register as a third party with NaviNet and follow the steps on the page.
General
If you are not registered for NaviNet please see our Provider Academy page.
For providers who do not belong to a PHO and are not a newly credentialed provider, please follow the steps below. Please note: The Provider Executive Team does not send fee schedules. To access fee schedules, please log in to NaviNet®.
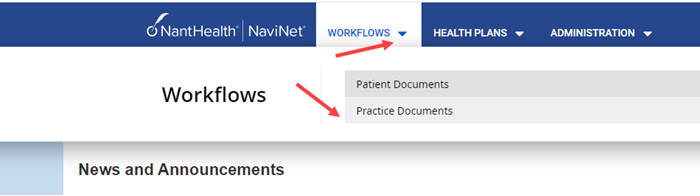
Your system administrator will need to give you access to Practice Documents. If they have any questions on how to do this, they will need to call NaviNet directly at 1-888-482-8057. If they already have, when you log in, under workflow you will need to click Practice Documents.
Your next steps will be to attest.

Once you attest you should be able to bring up the fee schedule. If you still cannot view your fee schedule, your system admin/security officer will need to change/update the user permission. It will state Security Office-User Permission and edit access and enable practice documents. If your system admin (or if you are the system admin) need assistance on this, please contact NaviNet directly at 1-888-482-8057.
NaviNet on new Windows 10 for Internet Explorer (or they can skip these steps and use Google Chrome):
- Go to the NaviNet login page.
- Prior to logging in, click the blue stop indicator in the URL line, between the lock and refresh.


- You’ll get a pop up, click “Turn off ActiveX Filtering”.
- This turns off the ActiveX Filtering for all downstream sites connected to the NaviNet login page. You’re all set!
Yes, all in-network providers, as well as the vendors supporting them, are required to use NaviNet for claims, benefits, and other questions.
If there are questions or concerns regarding member eligibility and claim status, please reach out to our Customer Service department at 800-635-0579.
For questions regarding logging in, access, setting up new users, or navigating the website, please reach out to NaviNet directly at 888-482-8057.
Benefits & Eligibility
Claim Status
Paid Claims
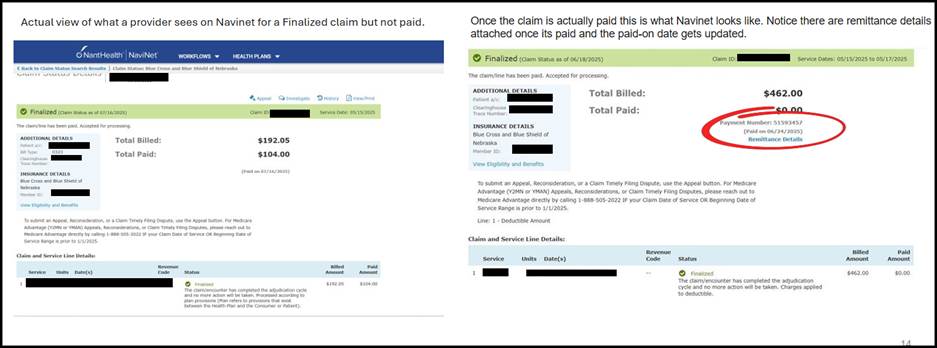
When a claim is finalized but payment has not been issued, NaviNet will display a “Paid on [date]” field without a hyperlink. This indicates the claim has completed processing but is still pending payment.
Once payment is issued, NaviNet will display the remittance details as a hyperlink. At that point:
- The hyperlink provides access to the full remittance information
- The “Paid on” date will update to reflect the actual payment date
Denied Claims
When looking at the claim in NaviNet, the detail is provided just above the claim-level information. It could be for another claim or another procedural code.
Non-Nebraska members claim denials are determined by the member’s plan and will not display in NaviNet.
The enhanced denial messages are exclusively available in NaviNet.
This will apply to claim denials for claim types: Professional, Institutional and Dental.
Enhanced messaging on claim denial reasons was added Dec. 29, 2023.
Please refer to your coder/biller for additional review prior to sending a claim investigation.
After performing a Claim Status Search, specific denial reasons will be shown for each denied claim line in Claim Status Details. Denial messages corresponding to the claim line number will be displayed directly above the Claim and Service Line Details.
